Lately, PRF is being marketed as the newest development in autologous biologics. The reality is that PRF has been around for as long as PRP and this is simply a rebranding by marketing departments to try and differentiate their companies product. In this article we will take a closer look so you can decide for yourself which product is right for you.
PRF
PRP is Platelet-Rich-Plasma, so what is PRF? The astute reader may have recognized that PRP and PRF both start with “PR”. This is not a coincidence! The PR in both stands for Platelet Rich. So then, it’s that last letter that really matters here. The “F” in PRF stands for Fibrin. PRF is Platelet-Rich-Fibrin.
What is Fibrin?
Fibrin is an insoluble protein that is formed from its precursor fibrinogen, a soluble protein that exists within blood plasma. This conversion of fibrinogen into fibrin is a key step in the coagulation cascade. It is catalyzed by the enzyme thrombin – which will be important to remember later. Once the fibrin molecules are created, they arrange themselves into a non-woven structure to form a stable clot over a wound site. Fibrin is the molecule that forms a clot.
Characteristics of PRP and PRF
So, the difference between PRP and PRF comes down to the medium within which the concentrated platelets are suspended and thus the handling characteristics of the final preparation. Plasma is a liquid that is easily flowable and can be adapted to procedures where that characteristic is required such as injections. Whereas fibrin is a clot resembling a solid gel that is not flowable and is much more suited to applications where a void would need to be filled.
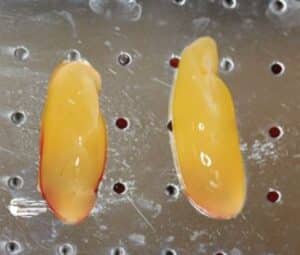
Traditional Application of PRF
Now that we’ve looked at the handling characteristics of PRF it is worth looking at one of its longstanding uses to get a better idea of its medical application. Dry socket is a painful dental condition that can occur after the extraction of a tooth, particularly the 3rd molar or “wisdom teeth”. This is caused by the blood clot that would normally form becoming dislodged or dissolving which exposes the underlying bone and nerve endings. PRF has been a solution to this issue. At the completion of the extraction the surgeon will prepare the PRF clot and place it directly into the socket. The PRF acts as a biological dressing with the added benefit of promoting tissue regeneration through the enrichment with platelets. In this instance PRP would not be a good solution since it is flowable. The socket is an open cavity, and any liquid would simply drain out. A fibrin clot on the other hand is a gel-like substance that can be filled into the void and will remain in place. In this instance PRF will be prepared by centrifuging blood without anti-coagulant. The results will be a fibrin plug that can be removed and used as discussed.
How is PRF Processed?
PRF is typically processed the same way that you process PRP; however, the clinician will either not add anticoagulant prior to spinning, or they will introduce thrombin to the finished PRP to catalyze the fibrinogen to form into a fibrin clot. In either case the result will be a platelet enriched clot, not suitable for flowable injection. This is the true distinction between PRP and PRF.
Is there a flowable PRF?
A true PRF is not a flowable Orthobiologic. That said, there are many companies that offer “PRF” product that is flowable, so what’s going on here? What they are really offering is PRP and calling it PRF. They do this in one of two ways through their protocols. The first way is to spin the whole blood without anti-coagulant; however, they spin it softly enough that the blood components separate but not hard enough to cause them to coagulate into a clot. There are two problems here. First, this will only be a single spin and at low force so you can imagine the concentration of platelets will be very low. Second, it doesn’t always work, and you will find yourself with a clot that can not be injected. A second advertised protocol is to add Calcium Chloride (CaCl) to a finished PRP and call this PRF. What does CaCl have to do with PRP? If you’re familiar with the PRP process, you know that an anti-coagulant is used to prevent coagulation during processing. Anti-coagulant works by binding and chelating calcium ions in the whole blood, which are crucial in the clotting cascade. Adding CaCl at the end of the process re-ionizes the calcium and it returns the blood back to its normal coagulation state. This does not cause the plasma to clot, so it doesn’t create any fibrin. You are still left with a flowable PRP, not a new product called PRF. There may be other “PRF” protocols out there, like heating the PRP or cooling the PRP, or agitating the PRP, the point is – if it doesn’t coagulate it’s still PRP. The answer to the question then is, no, there is no flowable PRF. You either have a gel like clot, called PRF or you have PRP (of potentially questionable quality – PRP quality classification) being called PRF as a marketing ploy based on protocols.
Can EmCyte PRP kits be used to make PRF?
Yes, however, remember that PRF is simply the platelet concentrate in a clotted form. So, in that case, any PRP kit can be used to make PRF. The question you need to ask yourself is, are you really looking for PRF? If you are intending to use a gel like clot, then you want PRF. If you want a flowable injectable, you want PRP.
Conclusion
We hope this article sheds some light on the differences (and similarities) between Platelet-Rich-Plasma and Platelet-Rich-Fibrin. One is not necessarily better than the other, it all comes down to handling characteristics and what your needs as a practitioner are.